Visit the data interactive
Racial Differences Among LGBT Adults in the US
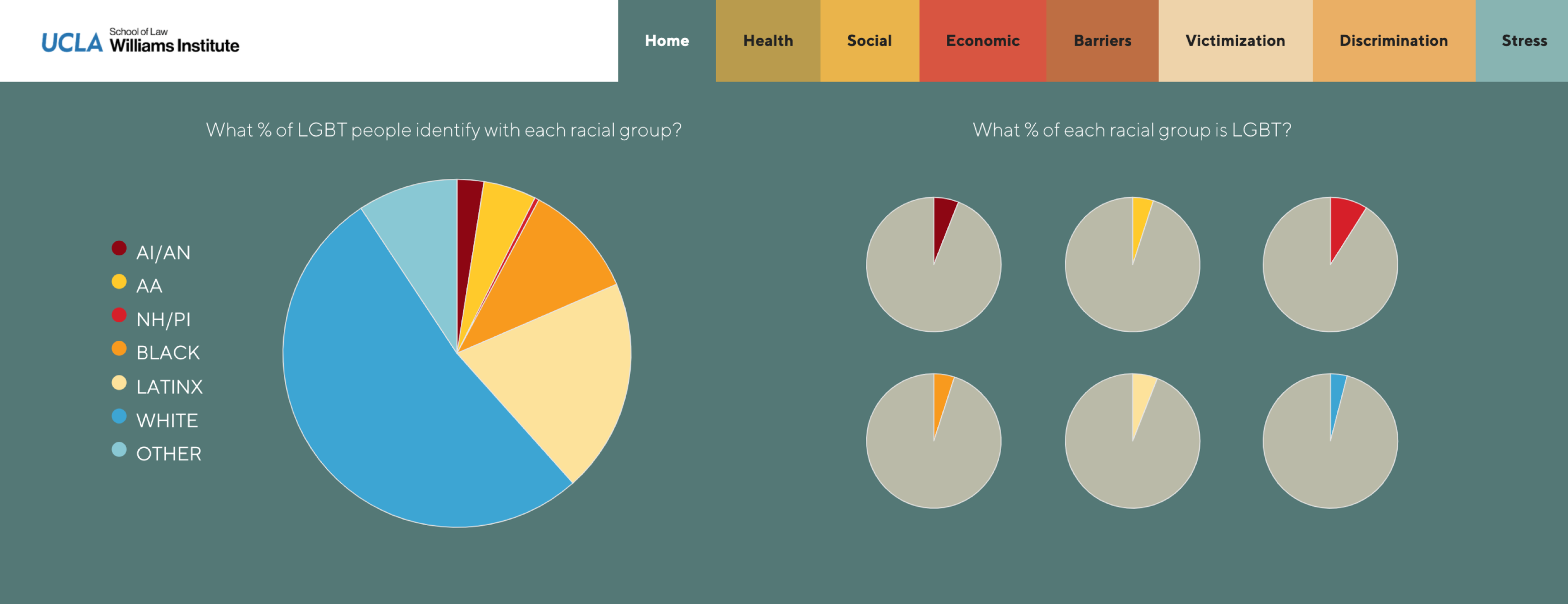
Using data from the Gallup Survey and the Generations and Transpop studies, this study examines whether adult LGBT people of color differ from White LGBT people in several areas of health and socioeconomic well-being.
Overview
This final report in the series, LGBT Well-Being at the Intersection of Race, uses data from the 2012-2017 Gallup Survey and the Generations/Transpop studies to assess whether LGBT people of color (POC) differ from White LGBT people on several areas of health and socioeconomic well-being. We find that more LGBT people of color report economic instability compared to White LGBT people on many indicators. Additionally, disparities for POC LGBT adults persist in the health domain, except for measures of depression where more White LGBT adults report having depression compared with POC LGBT adults. Further, more women of color who identify as LGBT reported living in a low-income household, and experiencing unemployment and food insecurity compared to all other groups. We also found differences in outcomes among LGBT POC on some economic and health indicators. Overall, the series of papers demonstrate that the relationship between race and LGBT status is a complicated one that differs by outcome and racialized group. Regardless of these complexities, the data point to the need for social and policy interventions that address economic and health disparities along racial, gender and LGBT statuses, separately and at their intersection.
Introduction
“No issue has proved more vexing to this nation than the issue of race.”
Race is arguably the most distinguishing factor delineating the U.S. population’s health,, economic state,, and freedom. Throughout the reports in this series, LGBT Well-Being at the Intersection of Race, we examine race and differences among LGBT adults by race, not as a biological characteristic, but as a social construct that has evolved in numerous ways in the U.S. in the interests of White supremacy. The previously published reports for this series provided data on the well-being of LGBT adults by racial groups in the U.S., with attention to areas in which sexual orientation and gender identity (SOGI) disparities may exist. Our previous analyses of whether there were differences between LGBT and non-LGBT adults within each racial group revealed a complex narrative on the role of LGBT status within racial groupings in the U.S. While White and Asian-American LGBT adults consistently fared significantly worse than their non-LGBT counterparts on economic and health indicators, the story was less consistent among other racialized groups. Those findings possibly point to the ways LGBT status varies as a driving force behind economic and health issues for racialized minority groups. This final brief in the series of reports on race and LGBT status adds to this work by synthesizing what the data show about the role of race among LGBT people in prevalence of economic, health, and social disparities.
White Privilege and LGBT Well-Being
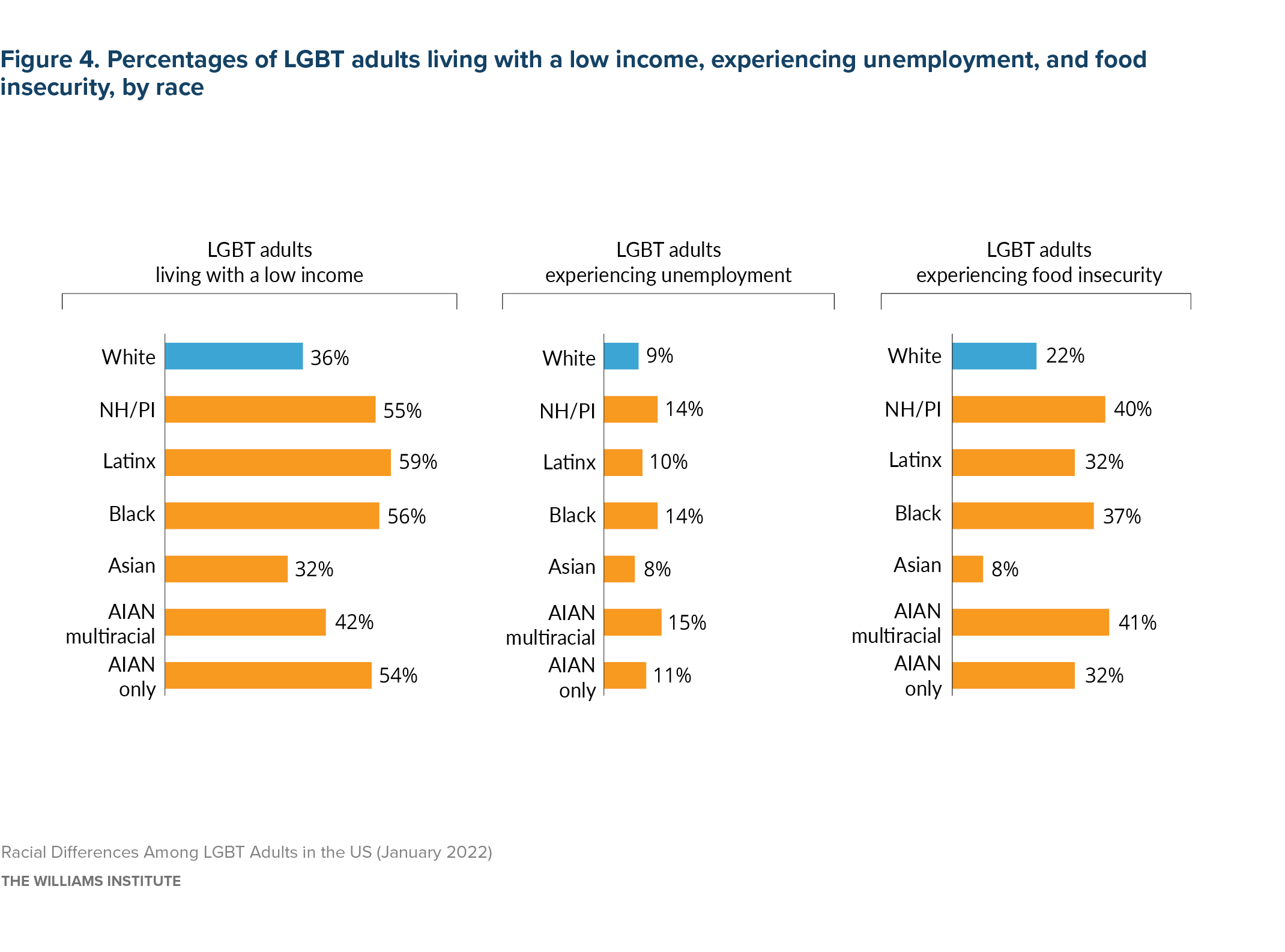
In most domains of health and social and economic well-being, LGBT people of color (POC) fared worse than White LGBT people. The analyses of economic outcomes show a consistent advantage experienced by White LGBT people. Fewer White than POC LGBT adults reported experiencing food insecurity, unemployment, use of Medicaid for health insurance, and living in a low-income household. For example, 47% of POC LGBT adults were living in a low-income household compared to 36% of White LGBT adults. Further, more women of color who identify as LGBT reported living in a low-income household and experiencing unemployment and food insecurity compared to all other groups.
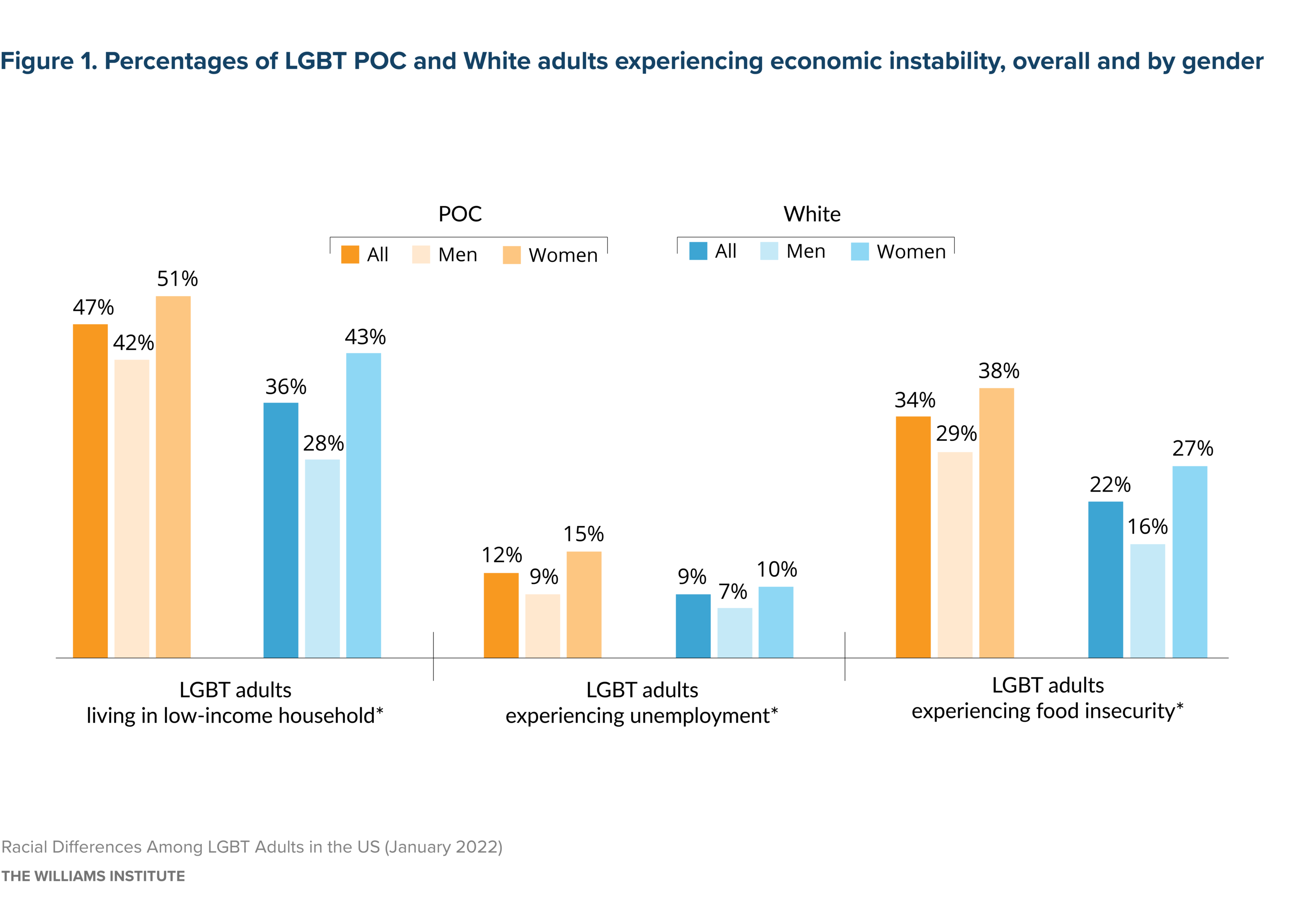
Source: Gallup, 2012-2017
Note: * indicates that estimates between LGBT POC and White LGBT adults (“All” group) are statistically different; POC includes respondents who identify as Asian/Asian American, American Indian or Alaska Native, Black, Latinx, Native Hawaiian or Pacific Islander, and Multiracial.
With regard to health, racial disparities among LGBT adults were identified in many domains, but not all. For example, more than a quarter (27%) of LGBT adults of color reported that their overall health was only fair or poor, compared to 22% of White LGBT adults. When looking across the specific health conditions (e.g., asthma, heart disease, diabetes, cancer), health behaviors (smoking, drinking), and stigmatized health factors (weight, disability) from the prior reports in the series, there is no consistent set of health factor differences across race among LGBT adults that may easily explain the higher percentage of fair and poor health reported by POC people.
Mental health is one domain of health outcomes in which racial minorities do not consistently fare worse than White respondents. Specifically, fewer POC LGBT adults report depression diagnoses compared to White LGBT people. This finding, particularly among Black Americans, is consistent with the general literature on racial differences in depression—while Black Americans tend to report higher levels of psychological distress than White Americans, they do not report depression diagnoses or symptoms at higher rates. Also in line with previous research, more women report experiencing depression than men, with White women reporting this most.
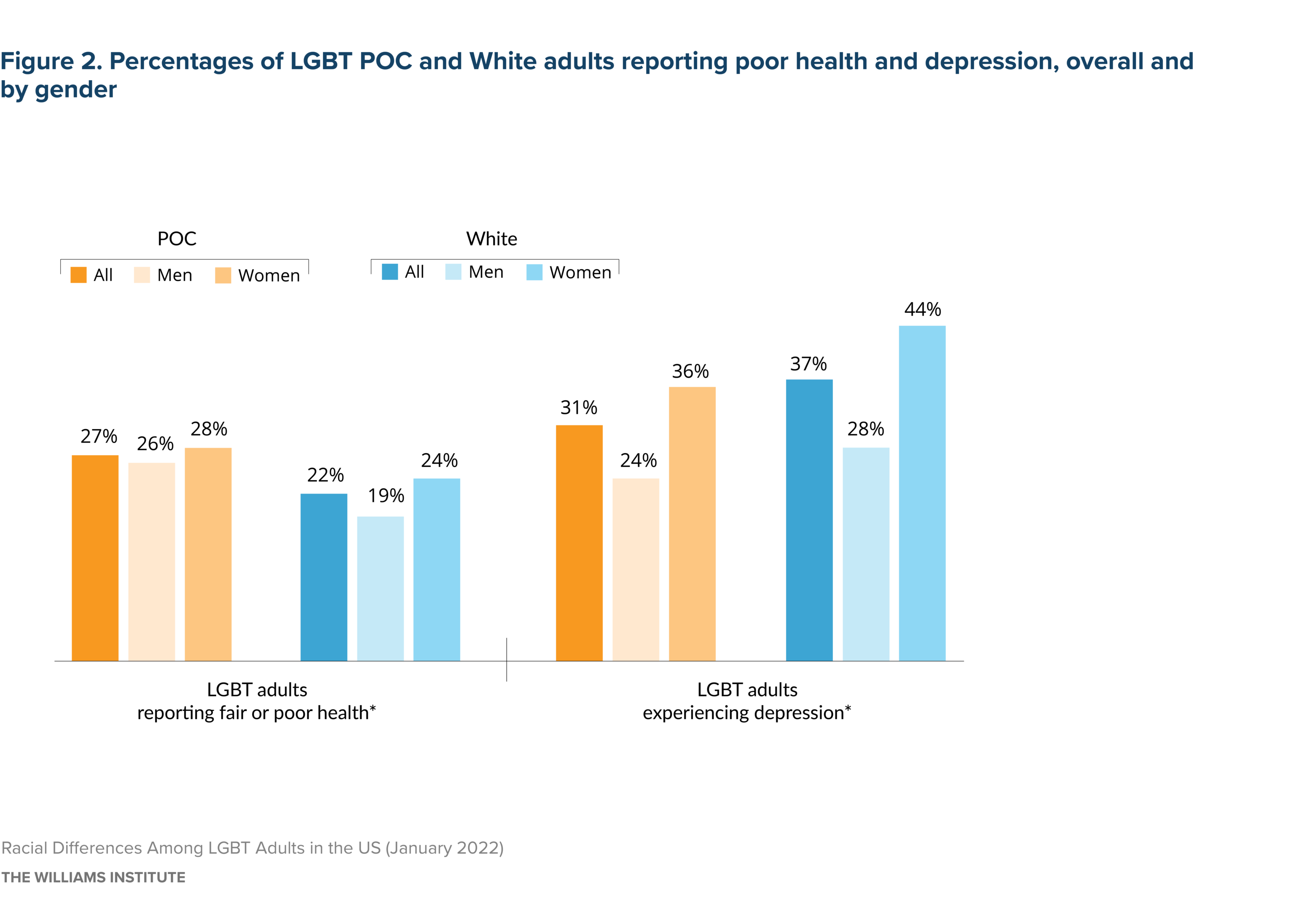
Source: Gallup, 2012-2017
Note: * indicates that estimates for POC LGBT and White LGBT (“All” group) are statistically different; POC includes respondents who identify as Asian/Asian American, American Indian or Alaska Native, Black, Latinx, Native Hawaiian or Pacific Islander, and Multiracial.
Diversity of Experience Among LGBT People of Color
Asian American LGBT people tend to have similar economic and often better health outcomes compared to White LGBT people, a finding that is reflected in the larger literature regardless of LGBT status. These findings also support current calls to disaggregate the data on Asian Americans and Native Hawaiians/Pacific Islanders in health and economic data reports as their experiences in the U.S. and outcomes remain very different. But there are other core differences among people of color that warrant highlighting. More American Indian and Alaskan Native (AIAN) LGBT adults report depression diagnoses than all other racialized groups. Also, among POC LGBT people, Latinx and Asian American people reported lower levels of unemployment than the other groups. Finally, AIAN and Latinx LGBT adults have among the highest rates of being uninsured for health care (see Table A2).
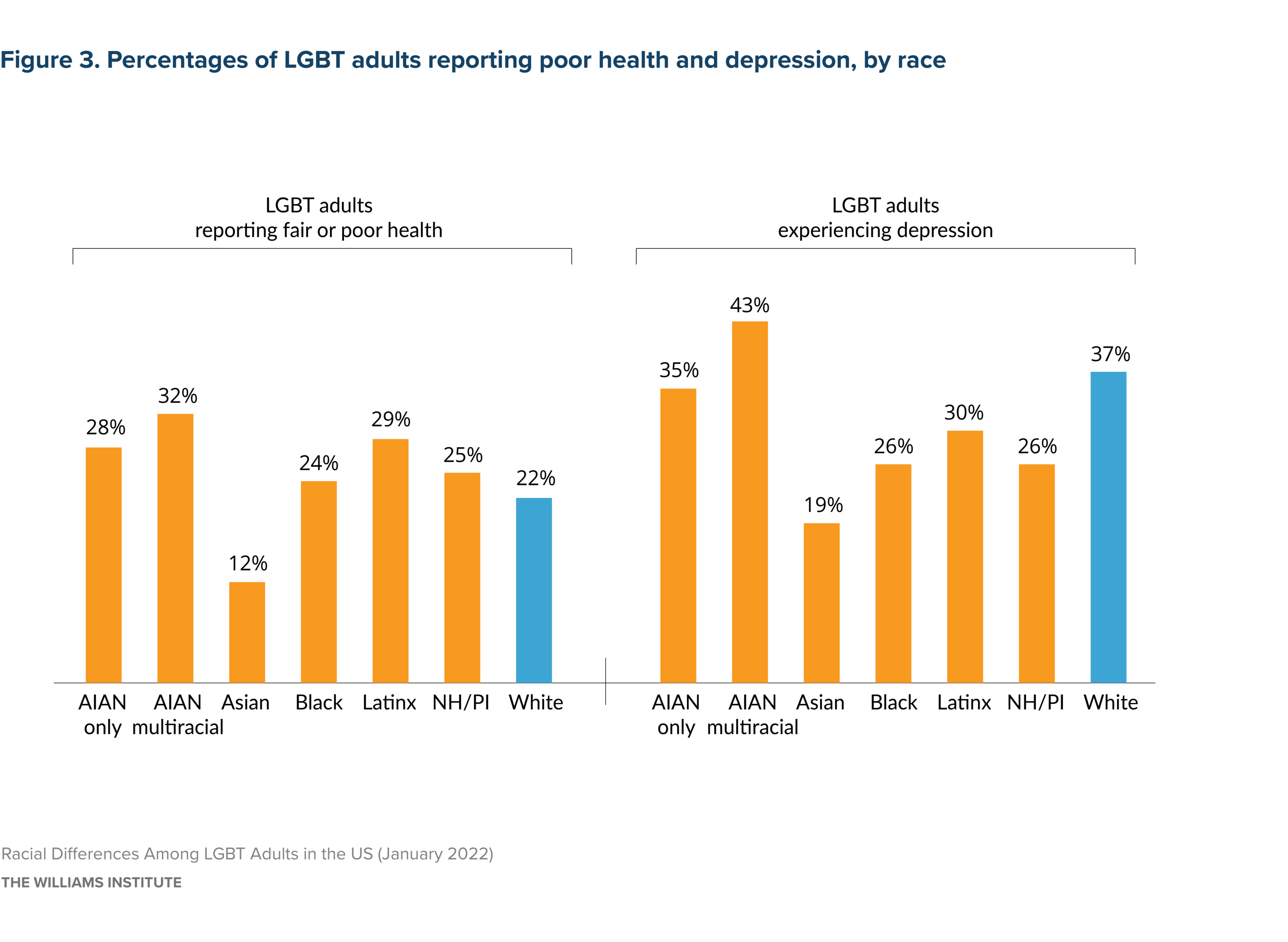
Source: Gallup, 2012-2017
Note: AIAN=American Indian/Alaska Native, NH/PI=Native Hawaiian/Pacific Islander
Source: Gallup, 2012-2017
Note: AIAN=American Indian/Alaska Native, NH/PI=Native Hawaiian/Pacific Islander
Considering Social Context when Examining Race and SOGI Disparities
As we have noted across the reports in these series, there are several core demographic and social life differences between LGBT and non-LGBT people that may be factors in the health and economic differences observed. There are similar differences in demographic and other characteristics across racial groups among LGBT people that could be relevant to understanding the impact of race on well-being. For example, more POC LGBT adults are under 30 years old, live in urban areas, and are single. Additionally, fewer POC LGBT adults have a college degree (25% vs 43%) and more report raising children (40% vs 22%) than White LGBT people. When gender differences are considered, more LGBT White men have college degrees and less of this group have children than all POC groups and White LGBT women (see Table A1).

Source: Gallup, 2012-2017
Note: * indicates that estimates between LGBT POC and White LGBT adults are statistically different.

Source: Gallup, 2012-2017
Note: * indicates that estimates between LGBT POC and White LGBT adults are statistically different.
Other social factors and experiences relevant to both health and economic well-being include experiences with employment and housing, as well chronic stress, discrimination, and victimization. In some areas, LGBT POC people fared worse than their White counterparts. For example, a higher percent of POC LGBT adults reported experiencing discrimination in the past year (78% vs 68%), a major financial crisis (35% vs 26%), and felt they were alone too much (56% vs 50%). However, both groups of LGBT adults reported relatively similar levels accounts of many other types of stressful experiences, including various forms of victimization and conflict with parents (see Table A2).
Considering LGBT Status, Race, and Intersectionality in Health and Well-Being
In this brief we demonstrated racial differences in well-being among LGBT adults—in ways that implicate the privilege of Whiteness that show differences among people of color. This report, along with the previous reports in this series demonstrating LGBT differences within racialized groups, highlight the ways sexual orientation, gender, and racial social statuses represent significant locations of inequities in the U.S. Further, findings from White LGBT Adults in the US indicate that White non-LGBT people, particularly men, report higher levels of well-being across most health and economic domains than all LGBT people. As such, the collection of reports in the series highlight evidence that White male heterosexual cisgender status remains a salient nexus of privilege.
Yet, the findings overall do not implicate a simplistic narrative of the impact of an intersectional marginalized social status on well-being. Though comparisons across the “SOGI x Race” diagonal (i.e., comparing White non-LGBT to POC LGBT) may appear to indicate a universalized intersectional oppression effect, an analysis of the many cases in which LGBT differences in well-being were small within some racial groups complicates those types of conclusions. For example, White and Black LGBT people consistently fared worse than their non-LGBT counterparts, but AAPI, AIAN and Latinx LGBT people often reported similar or better levels of economic stability and health than their non-LGBT counterparts. With regard to gender, LGBT women of color report higher rates of many mental health and economic outcomes than their male counterparts, but this is not always the case. Similar percentages of women and men of color who are LGBT report having overall poor or fair health, and all have higher than White LGBT men and women. Further, the percent of POC cisgender straight people living in a low-income household was typically higher than the percent reported by White LGBT people.
Taken together, the findings show that a focus on the ways LGBT people of color fare far worse than White non-LGBT people (the intersectional diagonal) partially masks the highly significant role that race plays among LGBT and non-LGBT people for most outcomes. It also has the potential to obscure the way LGBT status has an ever-salient role in understanding mental health disparities regardless of race. As part of informing an intersectional perspective to address inequities among oppressed groups, it is important for future research to continue highlighting the outcomes and indicators of well-being in which belonging to more than one marginalized group in the U.S. does or does not produce exponential disparities.
Alexander, M. (2020). The new Jim Crow: mass incarceration in the age of colorblindness, p. xvi. The New Press, New York, NY
Ford, C. (2019). Choosing a career in public health and a doctoral degree in sociology, and limitations of public health training. Racism: Science & Tools for the Public Health Professional (1st ed.). American Public Health Association. https://www.r2library.com/Resource/Title/0875533035/ch0003s0031
Bailey, Z. D., Krieger, N., Agénor, M., Graves, J., Linos, N., & Bassett, M. T. (2017). Structural racism and health inequities in the USA: evidence and interventions. The Lancet, 389 (10077): 1453–1463. https://doi.org/10.1016/S0140-6736(17)30569-X
Craemer T., Smith T., Harrison B., Logan T., Bellamy W., & Darity W. (2020). Wealth implications of slavery and racial discrimination for African American descendants of the enslaved. The Review of Black Political Economy, 47(3): 218-254. https://doi.org/10.1177/0034644620926516
Chetty, R., Hendren, N., Jones, M. R., & Porter, S. R. (2020). Race and economic opportunity in the United States: an intergenerational perspective. The Quarterly Journal of Economics, 135(2): 711–783. https://doi.org/10.1093/qje/qjz042
Alexander, M. (2010). The new Jim Crow: mass incarceration in the age of colorblindness. P. xvi. New York, NY: The New Press
Ford, C. (2019). Choosing a career in public health and a doctoral degree in sociology, and limitations of public health training. In Racism: Science & Tools for the Public Health Professional (1st ed.). American Public Health Association. https://www.r2library.com/Resource/Title/0875533035/ch0003s0031
We use the terms race and racial/ethnicity interchangeably throughout the report. We recognize that ethnicity specifically refers to a group bound by culture and sometimes nationality, and can be distinct from race as a social grouping and include racially diverse populations (Ford, C. L., & Harawa, N. T. (2010). A new conceptualization of ethnicity for social epidemiologic and health equity research. Social Science and Medicine, 71(2), 251–258. https://doi.org/10.1016/j.socscimed.2010.04.008). Yet, in the U.S., the ethnic groups we are including, adults of Latinx or Hispanic descent, Asian descent, and many Black subpopulations, in the U.S., they are treated socially and economically as racial groups (i.e., racialized) (Gómez, Laura E. 2020. Inventing Latinos: A New Story of American Racism. New York, NY: The New Press)
Wilson, B.D.M., Bouton, L., & Mallory, C. (2021). American Indian and Alaska Native LGBT Adults in the U.S. Los Angeles, CA: The Williams Institute, UCLA School of Law. https://williamsinstitute.law.ucla.edu/publications/aian-lgbt-adults-us/;
Wilson, B.D.M., Mallory, C., Bouton, L., & Choi, S.K. (2021). Latinx LGBT Adults in the U.S. Los Angeles, CA: The Williams Institute, UCLA School of Law. https://williamsinstitute.law.ucla.edu/publications/latinx-lgbt-adults-in-the-us/;
Choi, S.K., Wilson, B.D.M., Bouton, L. & Mallory, C. (2021). LGBT Asian American Pacific Islander Adults in the US: LGBT Well-Being at the Intersection of Race. Williams Institute: Los Angeles, CA. https://williamsinstitute.law.ucla.edu/publications/lgbt-aapi-adults-in-the-us/;
Choi, S.K., Wilson, B.D.M. & Mallory, C. (2021). Black LGBT Adults in the US. Williams Institute: Los Angeles, CA. https://williamsinstitute. law.ucla.edu/publications/black-lgbt-adults-in-the-us/;
Wilson, B.D.M., Bouton, L., & Mallory, C. (2021). White LGBT Adults in the US. Los Angeles, CA: The Williams Institute, UCLA School of Law. https://williamsinstitute.law.ucla.edu/publications/white-lgbt-adults-us/
Barnes, D. M., & Bates, L. M. (2017). Do racial patterns in psychological distress shed light on the Black-White depression paradox? A systematic review. Social psychiatry and psychiatric epidemiology, 52(8), 913–928. https://doi.org/10.1007/s00127-017-1394-9
Acciai, F., Noah, A. J., & Firebaugh, G. (2015). Pinpointing the sources of the Asian mortality advantage in the USA. Journal of epidemiology and community health, 69(10), 1006–1011. https://doi.org/10.1136/jech-2015-205623
Budiman, A, & Ruiz, N.G. (2021). Key facts about Asian origin groups in the U.S. Pew Research Center. Retrieved from; https://www.pewresearch.org/fact-tank/2021/04/29/key-facts-about-asian-origin-groups-in-the-u-s/. Accessed on December 14, 2021.
Tann, S. S., Yabiku, S. T., Okamoto, S. K., & Yanow, J. (2007). triADD: the risk for alcohol abuse, depression, and diabetes multimorbidity in the American Indian and Alaska Native populations. American Indian and Alaska native mental health research (Online), 14(1), 1–23. https://doi.org/10.5820/aian.1401.2007.5
See note, 9
See note, 9